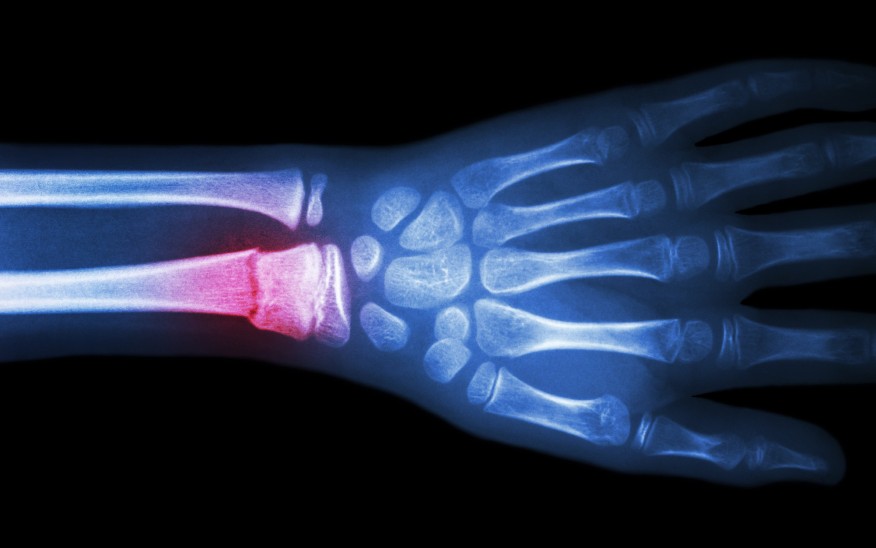
A distal radius fracture is commonly caused by what’s referred to as a FOOSH (Fall On Out Stretched Hand). In fact about 47% of distal forearm fractures are a result of a FOOSH and these also consist of about 44% of all upper extremity fractures (Cooper, 2015).
One of the most common distal radius fractures is the Colles’ fracture, where the distal end of the Radius is separated and forced dorsally. If the bone was fractured and forced towards the palm (volar) it would be called a Smith’s fracture (Cooper, 2015).
A benefit to this type of fracture is that it is relatively stable in most cases. Commonly treated by applying a simple wrist immobilization cast to ensure proper healing.

Sometimes the fracture is too unstable for just a splint. If the fracture isn’t stable as it will move too much for the body to properly reconstruct the fracture site.
If this occurs, then sometimes percutaneous pinning, casting, external fixation, and arthroscopic reduction are utilized (AAOS, n.d.).
The most common method for unstable fractures of the distal radius is by applying a metal plate to the bone to ensure stabilization. This helps ensure the bone maintains it’s proper length (fractures sometimes result in shortening of the bone). These plates can sometimes cause a period of tendon inflammation and reduced joint mobility during the rehabilitation process.
With wrist factures, there’s not always a guarantee that your full motion will return as it was before. That’s why it’s important to begin stretching as soon as it’s approved by your doctor or therapist. The benefits of these plate fixations, referred to as ORIF, is that it allows early active motion as soon as 1 week after surgery to prevent tissue adherence around the surgical site (Cooper, 2015). You’re surgeon will inform you of when they want you to start moving your wrist. If the fingers are free in the cast/brace, it’s safe to keep those gently moving as soon as you can unless otherwise directed.
Remember stretching and gentle movement is NOT strengthening!! Any added resistance (stress balls, weights) is considered strengthening. Strengthening is NOT recommended until around 8 weeks after the fracture or surgical intervention.
If the fracture site is not stabilized soon after the fracture occurs, this can result in a malunion. Where the bone heals misaligned. When this happens, the doctor and surgically repair this issue. If not, it can result in what’s considered Dinner Fork deformity, where the ulna is pushed toward the outside of the wrist. This can result in nerve impingement and soft tissue inflammation.
Sometimes, when strengthening begins, similar effects happen with tissue inflammation and swelling, but usually is addressed with manual therapy. Just because there’s some swelling, on the ulnar aspect of the wrist, doesn’t mean there’s a malunion. The bone callus formation can result in this as well.
FOR ONLINE COURSE RESOURCES, RECOMMENDED STRETCHES, EXERCISES, AND PROTOCOLS CLICK THE LINK BELOW!
Reference
AAOS. (n.d.). Distal Radius Fractures (Broken Wrist) – OrthoInfo – AAOS. OrthoInfo. https://orthoinfo.aaos.org/en/diseases–conditions/distal-radius-fractures-broken-wrist/.
Cooper, C. (2014). Fundamentals of hand therapy: Clinical reasoning and treatment guidelines for common diagnoses of the upper extremity (2nd edition). Elsevier Mosby.